
by Beju Shah, PharmD, MBA
Key takeaways
- Almost 10% of the US population with limited English proficiency (LEP) face language barriers in healthcare.
- The proposed rule, Section 1557 of the Affordable Care Act, aims to protect the rights of LEP individuals by all Section 1557 Notice of Proposed Rulemaking entities that receive federal funding.
- HHS Language Access Plan guides federal agencies in improving LEP access through interpreters and translation services.
Healthcare professionals in the United States face a common problem. They need to provide appropriate medical care, but when there is a language barrier, it can pose a significant obstacle. In this article, we will cover the key implications of the proposed rules for section 1557 of the Affordable Care Act (ACA) and the recent updates to the federal language access plan.
To get started, let’s take a look at a common scenario that showcases why language access is important.
Scenario: Mrs. Rodriguez, a 75-year-old immigrant from Mexico, arrives at a clinic seeking medical care. She is visibly distressed and in need of attention. Unfortunately, she faces a language barrier as she is not fluent in English. As Mrs. Rodriguez approaches the front desk, she tries to express her symptoms, pointing to her chest and mentioning words like "dolor" (pain) and "cansancio" (fatigue). In the waiting room, she is surrounded by English-speaking staff and patients, creating an environment where communication becomes a significant challenge. The receptionist, while well-intentioned, struggles to understand her due to the language difference. As Mrs. Rodriguez struggles to communicate her symptoms and understand staff instructions, she is left feeling frustrated and misunderstood.
Problem: She was eventually seen by a provider, but the delayed intake may have impacted the overall patient experience. This situation highlights a common issue in healthcare—the lack of effective communication with patients of limited English proficiency.
Ideal solution: To assist patients like Mrs. Rodriguez, access to medical interpreters for real-time communication and cultural competence training for healthcare professionals would be helpful to ensure effective communication, addressing the specific needs of patients with limited English proficiency.
The reality is that almost 10% of people aged five or older in the United States have limited English proficiency (LEP). Timely access to language assistance is crucial in addressing their health coverage access and enhancing the quality of care. These patients often face disproportionate gaps in care. Given the significant number of Americans speaking a language other than English at home, healthcare providers must prioritize integrating interpretation and translation services. This not only aligns with ethical considerations but may also be mandatory under federal regulations.
The importance of language accessibility
Communication is a critical step in the continuum of care for patient safety—from informed consent to follow-up visits. Research shows that patients with LEP have a greater risk than their English-proficient counterparts of adverse events when a language barrier exists. However, when patients understand the conversation, they're more likely to have positive outcomes. Simply put, every patient deserves to receive information in a way that makes sense to them.

Scenario: Sanjay, a concerned father with limited English proficiency, took his 8-year-old son, Ashok, to the local clinic after noticing recurrent wheezing and difficulty breathing. The clinic diagnosed Ashok with asthma and prescribed an inhaled corticosteroid as a preventive measure to manage the condition. The healthcare provider explained the importance of using the inhaler daily to prevent asthma attacks and control symptoms. However, overwhelmed by the new diagnosis and language barriers, Sanjay struggled to fully understand the instructions and assumed the inhaler was only for emergencies, not realizing its daily use was important.
Problem: Due to the language barrier and misinterpretation of the instructions, Sanjay administered the inhaled corticosteroid to Ashok only when he noticed severe symptoms or during asthma attacks. This misunderstanding led to inadequate control of Ashok's asthma. They ended up relying on quick-relief medications. They had frequent emergency room visits and noticed a decline in Ashok's overall well-being. The failure to comprehend the prescribed daily regimen significantly impacted the effectiveness of the asthma management plan, highlighting the challenges faced by individuals with limited English proficiency.
Ideal solution: Encouraging questions and providing written instructions in the patient's preferred language can help individuals like Sanjay comprehend the preventive nature of the medication and the importance of consistent daily use. Visual aids, like whiteboard instructions, can also enhance understanding, especially for those with limited English proficiency. By tailoring communication to accommodate language barriers, healthcare providers can empower fathers like Sanjay to effectively manage their child's treatment.
Let's dive into the resources and strategies that can enhance language access in telehealth.
Brief background on federal regulations
It’s important to understand the changes in policy, as they could have a significant impact on staying compliant with federal regulations. Here are key highlights to review for your program.
Proposed rules with the Affordable Care Act
On August 4, 2022, the US Department of Health and Human Services (HHS) proposed a rule to enhance civil rights protections in federally funded health programs. When this new rule, related to Section 1557 of the ACA, is finalized, it will advance health equity.
This federal mandate underlines that no individual participating in, benefiting from, or engaging in any health program or activity receiving federal financial assistance should face exclusion, denial of benefits, or discrimination. It explicitly forbids discriminating against individuals with limited English proficiency.
Expanding on nondiscrimination protections
The proposed rule seeks to expand on existing provisions while also introducing new policies. Here are five key elements that you should be aware of:
- Expanded coverage: The mandate would cover the entire business of each entity, not just the parts that receive federal funds. Ultimately, this would broaden the scope of insurers, healthcare entities, and HHS health programs and activities.
- Extension to Medicare Part B: The mandate would also be applied to Medicare Part B payments, which currently exempt physicians and other outpatient providers (unless they receive federal funds from other sources).
- Notification of rights: Organizations would be required to inform individuals about the availability of language assistance services.
- Compliance training: Organizations would be required to adopt specific policies and procedures. Employee training on these new standards would be mandatory.
- Clinical decision support: The rule would prohibit covered entities from discriminating through clinical algorithms in healthcare decision-making and the delivery of telehealth services.
While Section 1557 is still subject to further review and potential legal challenges, its introduction comes at a crucial time when the COVID-19 pandemic has highlighted significant inequities in healthcare.
Federal updates to the Language Access Plan
On November 15, 2023, the HHS released its updated Language Access Plan to enhance access for the LEP community and individuals with disabilities. This plan provides practical guidance, best practices, and action steps for federal agencies to develop their access plans. As healthcare providers anticipate the release of the final rule, these updates serve as a preview of potential developments and offer guidance on implementing compliance plans.
The plan covers ways to improve access, including:
- Digital information: Websites are available in more languages than just English.
- Interpretation services: Provide telephone, video, or virtual interpreting services (including visual/auditory disability accommodations).
- Written translations: Provide program and benefit details in languages other than English.
- Policies and procedures: Align internal resources with national standards.
- Training: Staff have access to relevant resources and training.
3 key tips that can advance your program
If providing these resources seems like a difficult task, these tips will help. Here are some easy, practical ways you can improve language accessibility today.
Interpreter services
Healthcare professionals sometimes use family members or bilingual staff to “get by” during a session, often for convenience or as a cost-effective measure. However, it's crucial to remember that qualified training is essential for accurate interpretation. To implement language support, consider outsourcing professional interpreter services.
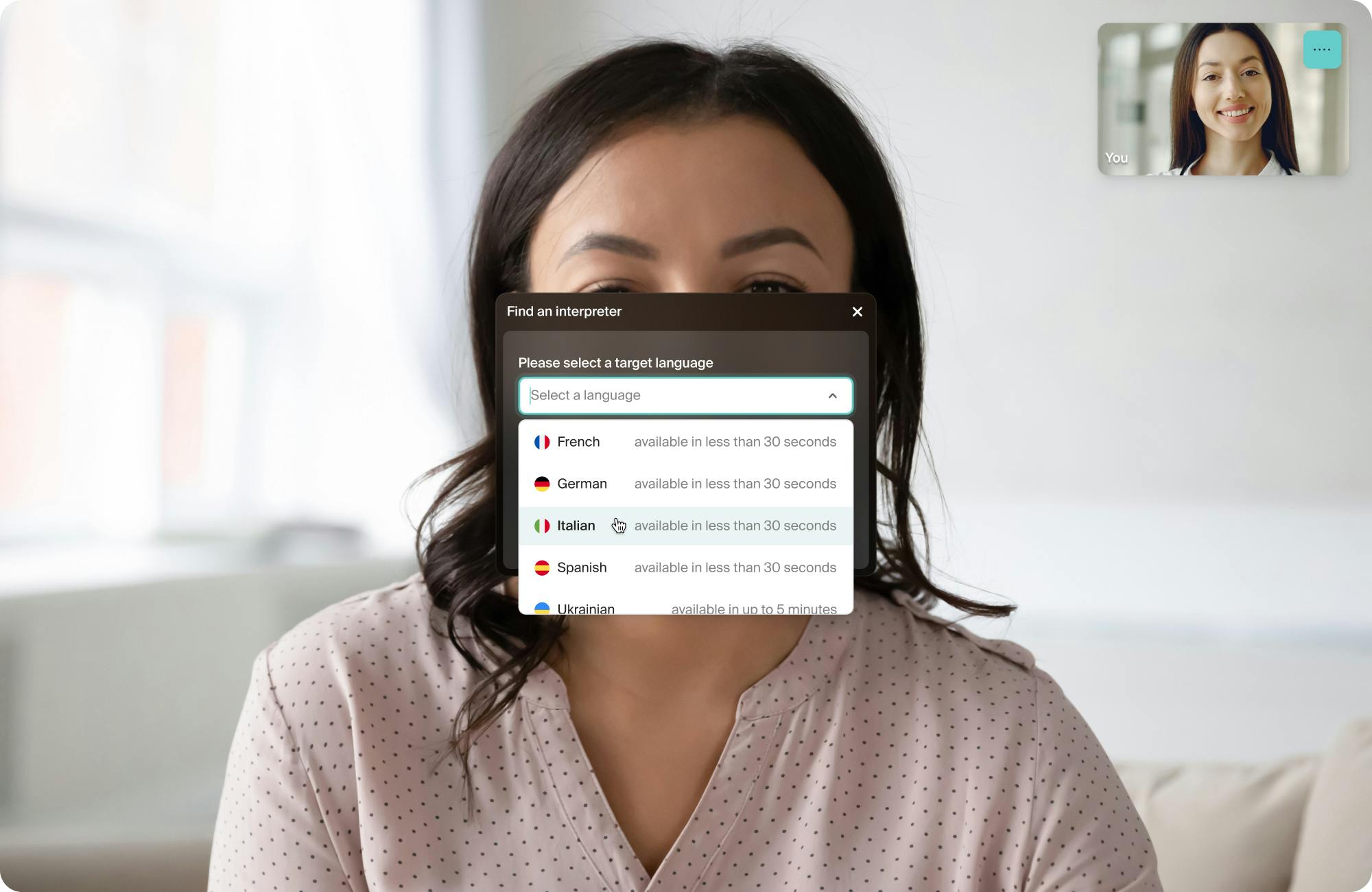
Integrating consistent video interpretation into the daily workflow can build rapport with the patients, family members, or advocates, even for small interactions. An on-demand interpreter can help create a frictionless workflow. On-demand interpreters can reduce work for your team since there’s no scheduling needed.
Doxy.me’s on-demand solution has over 70 languages, including American Sign Language (ASL), with professional interpreters trained to industry standards.
Group calls
By launching virtual group calls, healthcare professionals can enhance family-centered rounds and improve patient care. Instead of relying on family members as interpreters, involve them directly in the patient's care. Family-centered rounds with a multidisciplinary team can impact family understanding, care coordination, and medical education. It also addresses the importance of interpreting side conversations among clinical staff, which can provide comprehensive information to patients and their families or advocates.

Multilingual patient information and consent forms
Outside of visits, don’t forget to provide resources in patients’ preferred languages. Here are a few types of information every practice should consider when thinking about language accessibility.
Educational materials
Healthcare organizations should provide patient education materials in multiple languages to ensure patients understand medical conditions, treatment plans, and medication instructions.
Consent forms
Customize consent forms to accommodate other languages and obtain a patient's digital signature for participation in telehealth appointments. If you seek options beyond the standard teleconsent form, consider opting for a Professional, Clinic, or Enterprise account.
(Meet three nonprofits that are increasing access to healthcare—one of which uses custom consent forms.)
Website
Your website should support multiple languages, and you can set a default language by configuring the browser settings. In fact, doxy.me supports over 100 languages for patients and will automatically appear in that language.
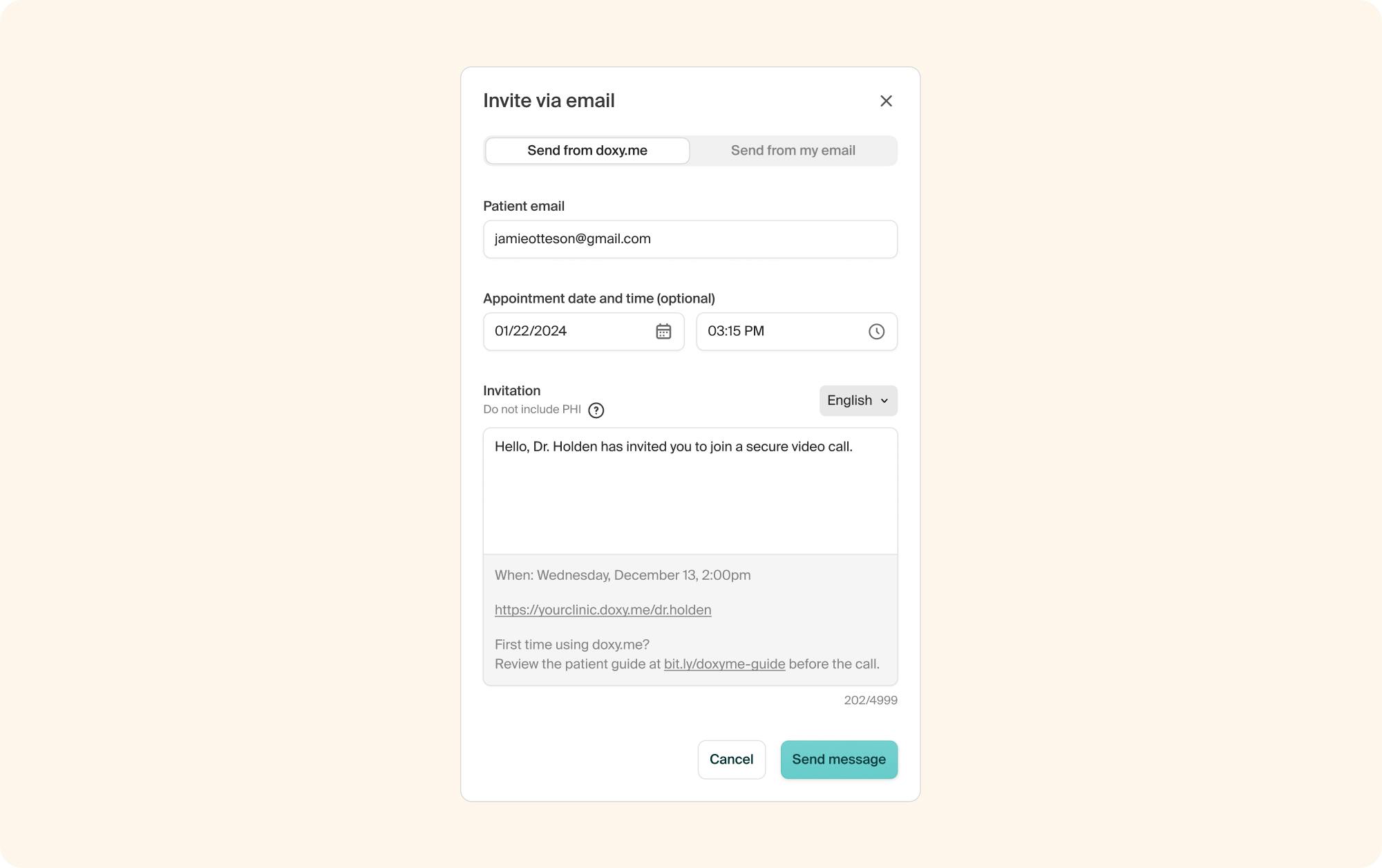
Scheduling invites
Scheduling patient invitations in their language is an important step in ensuring follow-up care. With doxy.me, you can send patient invites in 22 different languages using the language selector.
Reminder: Always have qualified human translators review machine-translated materials, especially when accuracy is crucial, or the source material is complex or technical.
Start improving healthcare equity
The language access plans launched by federal agencies, particularly the HHS Language Access Plan, emphasize the importance of promoting inclusivity in healthcare. Telehealth can be a convenient way to improve access and remove language barriers. By incorporating these resources and strategies into telehealth practices, you can help create a healthcare system that is inclusive, accessible, and equitable for all individuals—regardless of their language proficiency.